Types and Applications of Rubber Stoppers in Pharmaceutical Packaging
Pharmaceutical rubber stoppers serve as critical sealing components across drug packaging formats. Their design variations address distinct functional requirements in containment and drug delivery systems.
Serum vs. Lyophilization Stoppers: Functional Differences
- Lyophilization stoppers feature vents or permeable materials to allow moisture escape during freeze-drying processes, with 87% of lyophilized drug products using vented designs (Pharmaceutical Packaging Report 2023).
- Serum stoppers prioritize needle resealability, using thicker elastomer layers (6–8 mm) to maintain seal integrity after 10+ punctures in IV bag applications.
Rubber Stoppers for Pre-Filled Syringes and Cartridge Seals
Pre-filled syringe systems utilize bromobutyl rubber stoppers for their low moisture permeability (≈0.1 g/m²/day) and compatibility with biologics. Cartridge seals for auto-injectors require compression forces ≈35 N to ensure smooth plunger movement while preventing backflow, per USP <1382> guidelines on injectable packaging.
Application in Vaccines, Biologics, and Diagnostic Products
Vaccine vial stoppers account for 32% of pharmaceutical rubber component demand (Global Market Insights 2024), driven by requirements for:
- Trace metal levels <1 ppm in COVID-19 mRNA vaccines
- Gamma irradiation stability for single-dose biologics
- Optical clarity in diagnostic reagent containers
Role of Rubber Stoppers in Injectable Drug Packaging Systems
Injectable drugs rely on stoppers to maintain sterility across 90% of parenteral products. Critical performance metrics include:
- ≈0.05% leakage rates during transport (EMA 2023 stability mandates)
- 0.22 µm particulate filtration efficiency
- ≈0.3% compression set after 72-hour sterilization cycles
This functional specialization enables rubber stoppers to meet evolving regulatory standards while addressing diverse drug formulation needs.
Material Composition and Chemical Compatibility of Rubber Stoppers
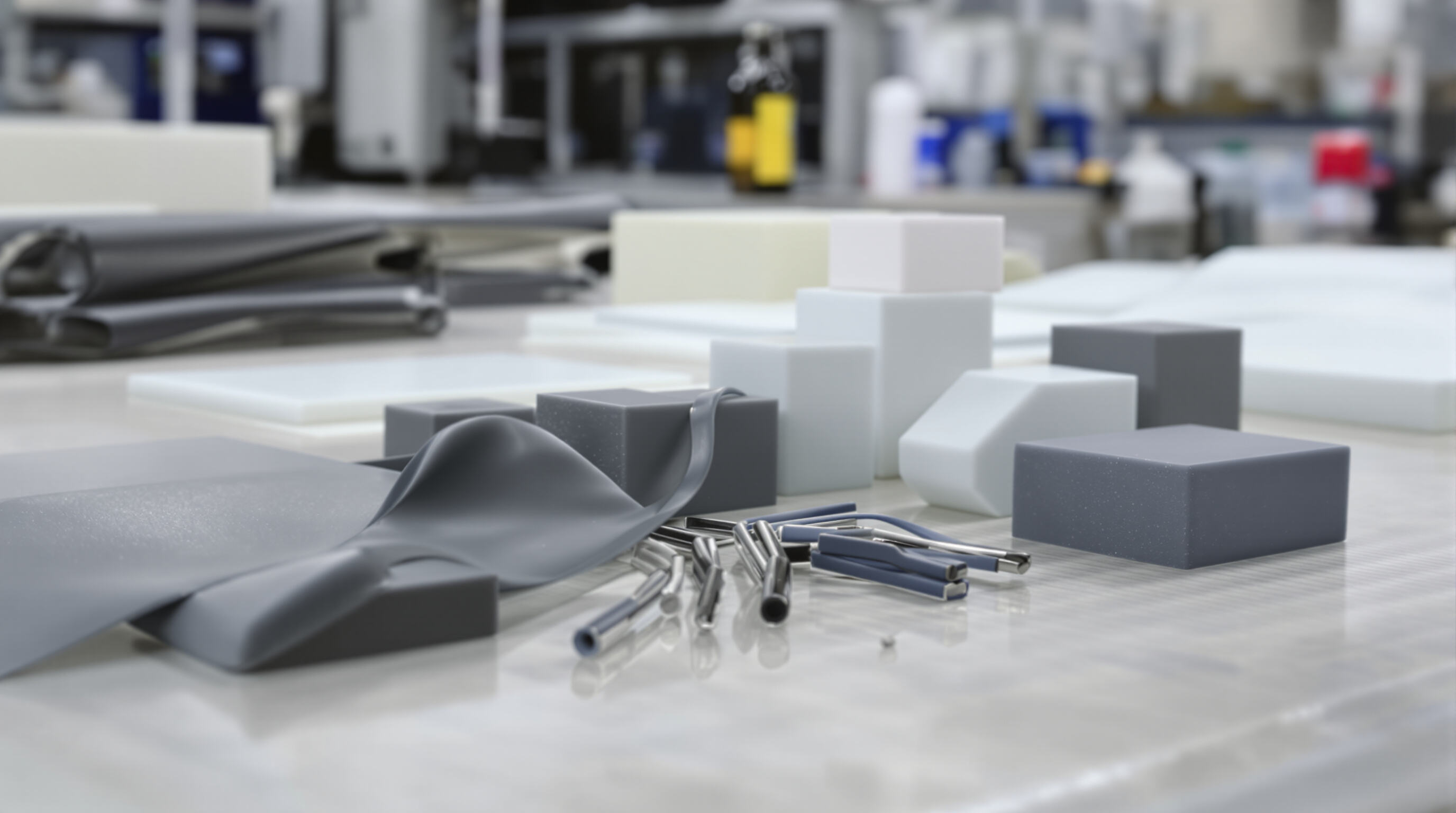
Butyl Rubber, EPDM, and Silicone: Comparing Material Types Used in Pharmaceutical Stoppers
In pharmaceutical stopper manufacturing, three main types of rubber are commonly used. Butyl rubber stands out because it doesn't let gases pass through easily, which is why most vaccines come sealed with this material. The industry really favors butyl rubber for vaccine packaging since it creates such a good moisture barrier. This helps protect sensitive biological products from breaking down, cutting hydrolysis risks anywhere from 60 to 80 percent better than regular natural rubber does. Then there's EPDM rubber, known scientifically as Ethylene Propylene Diene Monomer. What makes EPDM special is how well it holds up against steam at temperatures reaching 150 degrees Celsius, so it works great for those freeze-dried medication containers. And finally we have silicone, which performs exceptionally well in both extremely cold and hot conditions ranging from minus 80 all the way up to 250 degrees Celsius. That's why silicone is often found in auto injectors and prefilled syringes where needles puncture the seal but still need to maintain integrity afterward. Tests show that silicone seals can be closed again successfully about 97 times after being pierced once.
Chemical Compatibility Between Rubber Stopper Materials and Drug Formulations
When materials don't play nice with drugs, it really affects how stable the final product stays. Some rubber components actually release sulfur stuff or other small molecules into liquid medications when they're not compatible. According to research published last year, nearly half (around 42%) of all recalled medicines had problems related to stoppers causing changes in pH levels beyond what's acceptable for buffered solutions. The good news is newer versions of halogenated butyl rubber bring down these unwanted substances to below 0.5 micrograms per milliliter. This improvement has been checked using special tests outlined in USP chapter 381 which looks at oxidation risks specifically for biological products and those tricky mRNA vaccines we've heard so much about lately.
Impact of Additives and Curing Agents on Material Performance
Plasticizers like dioctyl phthalate improve elastomer flexibility but increase leachable risks by 30% in lipid-based drugs. Peroxide curing systems, while generating fewer nitrosamines than sulfur-cured alternatives, require strict control of residual methyl ethyl ketone (<10 ppm) under EMA guidelines.
Halogenated vs. Non-Halogenated Polymers: Safety and Performance Trade-offs
Chlorobutyl variants demonstrate 5x higher chloride-ion resistance than brominated analogs, crucial for saline-based infusions. However, non-halogenated grades meet USP Class VI biocompatibility standards with a 99.9% reduction in volatile organic compounds, preferred for long-term biologic storage.
Critical Physical Properties and Sealing Performance of Rubber Stoppers

Hardness, Elasticity, and Tensile Strength in Sealing Efficacy
The right balance of properties is essential for rubber stoppers used in pharmaceutical vials. They need to have a certain hardness range around Shore A 40 to 60, plus good elasticity with at least 300% elongation capability, and sufficient tensile strength above 15 MPa to keep the seal intact. The harder the compound tends to be, the better it resists coring when needles go through them. Elasticity matters too because it allows the rubber to bounce back after being compressed. Studies show that when rubber has optimal tensile strength, it actually cuts down on particulate formation by roughly 60 something percent during multiple punctures compared to lower quality alternatives. Take the latest findings from the 2024 Pharmaceutical Material Performance Report for example they found thicker rubber layers can boost sealing force about 19% in those freeze dried drug products where maintaining vacuum conditions is so critical.
Compression Set and Re-Sealability After Needle Penetration
Getting compression set values under 25% after sitting at 70 degrees Celsius for around 22 hours is pretty important if we want those stoppers to keep sealing properly in multi dose vials. The problem comes when stoppers don't hold up well under pressure they tend to lose about 38% of what makes them seal tight after just three times getting poked by needles, which opens the door for microbes to sneak in. Fortunately, newer halogenated butyl materials have shown amazing results, keeping leakage below half a percent even after being pierced five times. These numbers check off the requirements set out in USP chapter 1381 for packaging injectables, so manufacturers know they're on solid ground with these materials.
Case Study: Performance Testing of Stoppers Under Repeated Use Conditions
A 2021 nonlinear finite element analysis tested over 1,000 puncture cycles across stopper types. Silicone stoppers showed 58% faster seal degradation than bromobutyl variants, correlating with their lower tensile strength (12.7 MPa vs. 18.3 MPa). Post-test chemical analysis revealed thermoplastic elastomers maintained sterility with <0.1% moisture permeability, proving essential for biologics requiring extended shelf lives.
Ensuring Sterility, Integrity, and Regulatory Compliance
Moisture and Gas Permeability in Vial Seals and Long-Term Stability
Rubber stoppers play a vital role in parenteral drug packaging by stopping moisture from getting in and preventing unwanted gas exchange, which helps keep drugs stable over time. When it comes to specific materials, butyl rubber stops moisture pretty effectively with permeability rates under 0.1 grams per square meter per day. Some special halogenated compounds go even further, cutting down oxygen transmission to less than 3 cubic centimeters per square meter daily. These numbers actually meet the standards set out in ICH Q1A guidelines for things like biologics and vaccines. Manufacturers care about these specs because they directly impact how long medications stay effective after production.
Ensuring Sterility Through Effective Rubber Stopper Sealing
Compression-resistant elastomers create microbial barriers exceeding ISO 14644-1 Class 5 cleanroom standards. Post-sterilization sealing performance is validated through microbial ingress testing per USP <1207>, with modern stoppers demonstrating zero contamination rates in 99.97% of simulated 14-day challenge tests.
FDA, EMA, and USP Requirements for Rubber Stopper Qualification
Regulatory bodies mandate:
- FDA 21 CFR 211.94: Material compatibility documentation for drug-contact surfaces
- EU GMP Annex 1 (2023): Vial closure system validation under worst-case storage conditions
- USP <382>: Elastomeric closure functionality testing for seal integrity
Manufacturers must provide extractables profiles meeting ICH Q3D elemental impurity thresholds across all material grades.
Sterilization Requirements for Rubber Stoppers in Aseptic Manufacturing
Gamma-irradiated stoppers maintain sterility assurance levels (SAL) of 10⁻⁶ after processing at 25–40 kGy doses. For terminal sterilization, autoclave-resistant formulations withstand 121°C/15 psi cycles without deformation. Steam-In-Place (SIP) validation requires three consecutive successful batch tests under FDA Process Validation Guidance (2024).
Extractables, Leachables, and Emerging Market Trends
Understanding Extractables and Leachables in Rubber Stoppers
The presence of extractables (those chemicals that come out when exposed to harsh conditions) and leachables (materials that migrate into products during normal use) continues to be a major issue for rubber stopper quality control. Research published last year showed something quite concerning actually - if manufacturers don't choose their materials carefully, there's about a 23 percent higher risk of contamination problems showing up in biological drug preparations. The USP has put forward specific standards in document number 1663 that require thorough analysis of both types of substances. These tests are necessary because many modern medications, including those monoclonal antibody treatments, simply cannot tolerate even small amounts of foreign chemical interference.
Testing Procedures for Rubber Stoppers Under USP <1663> Guidelines
The USP <1663> framework requires three-stage testing:
| Stage | Objective | Analytical Methods |
|---|---|---|
| 1 | Extractables profiling | GC-MS, LC-MS, FTIR |
| 2 | Simulated leachables study | Accelerated aging tests |
| 3 | Real-time migration monitoring | ICP-MS for metal ions |
Manufacturers must achieve detection limits below 0.1 ppm for high-risk contaminants like nitrosamines.
Risk Mitigation Strategies for Contamination in Biologics
Material reformulation reduces extractables by 40–60% in advanced halobutyl rubber grades. A 2022 case study demonstrated that applying fluoropolymer barrier films on stoppers lowered leachable levels by 72% in vaccine vials. Predictive modeling tools now enable 85% accuracy in forecasting chemical interactions between stoppers and pH-sensitive biologics.
Rising Demand for Injectable Drugs and Biologics as Market Drivers
The global injectable drug market, projected to reach $987.2 billion by 2027 (7.1% CAGR), directly amplifies rubber stopper requirements. Biologics alone account for 38% of pre-filled syringe component demand, driving innovation in ultra-clean stopper manufacturing. Emerging mRNA vaccine platforms further necessitate stoppers with <0.01% moisture permeability to maintain lyophilized product stability.
FAQs
What are the key differences between serum and lyophilization stoppers?
Serum stoppers prioritize needle resealability using thicker elastomer layers to maintain seal integrity after multiple punctures, while lyophilization stoppers have vents to allow moisture escape during freeze-drying.
Why are bromobutyl rubber stoppers used in pre-filled syringes?
Bromobutyl rubber stoppers are used in pre-filled syringes due to their low moisture permeability and compatibility with biologics, ensuring drug stability and safety.
What are the primary materials used in rubber stopper manufacturing?
The main materials used in rubber stopper manufacturing include butyl rubber for its moisture barrier properties, EPDM for thermal resistance, and silicone for temperature extremes.
Why is chemical compatibility important for rubber stoppers?
Chemical compatibility is vital because incompatible rubber components may release harmful substances into drugs, affecting their stability and safety.
What testing procedures are involved in ensuring the quality of rubber stoppers under USP <1663> guidelines?
The USP <1663> guidelines require a three-stage testing process involving extractables profiling, simulated leachables studies, and real-time migration monitoring to ensure the safety of rubber stoppers.
Table of Contents
- Types and Applications of Rubber Stoppers in Pharmaceutical Packaging
-
Material Composition and Chemical Compatibility of Rubber Stoppers
- Butyl Rubber, EPDM, and Silicone: Comparing Material Types Used in Pharmaceutical Stoppers
- Chemical Compatibility Between Rubber Stopper Materials and Drug Formulations
- Impact of Additives and Curing Agents on Material Performance
- Halogenated vs. Non-Halogenated Polymers: Safety and Performance Trade-offs
- Critical Physical Properties and Sealing Performance of Rubber Stoppers
- Ensuring Sterility, Integrity, and Regulatory Compliance
-
Extractables, Leachables, and Emerging Market Trends
- Understanding Extractables and Leachables in Rubber Stoppers
- Testing Procedures for Rubber Stoppers Under USP <1663> Guidelines
- Risk Mitigation Strategies for Contamination in Biologics
- Rising Demand for Injectable Drugs and Biologics as Market Drivers
- FAQs
- What are the key differences between serum and lyophilization stoppers?
- Why are bromobutyl rubber stoppers used in pre-filled syringes?
- What are the primary materials used in rubber stopper manufacturing?
- Why is chemical compatibility important for rubber stoppers?
- What testing procedures are involved in ensuring the quality of rubber stoppers under USP <1663> guidelines?







